Abstract
Background: MYD88 mutation, especially the Leu 265 Pro (L265P) variant, has been widely reported to act as an oncogenic driver in diffuse large B-cell lymphoma (DLBCL). However, for other mutation variants of MYD88, it remains largely unknown on their difference with the MYD88 L265P variant. Therefore, we aim to investigate the molecular differences of MYD88 L265P mutation and other variants in DLBCL patients treated with R-CHOP in China using retrospective analysis.
Methods: We collected definitely diagnosed DLBCL patients with MYD88 mutation information at the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, and Suzhou Municipal Hospital from February 6th, 2007 to May 20th, 2022. Immunohistochemistry was used for evaluating the protein expression, while capture-based targeted sequencing and fluorescence in situ hybridization were adopted for detecting genetic alterations. Chi-squared test or Fisher's exact test was adopted for the comparisons between categorical variables.
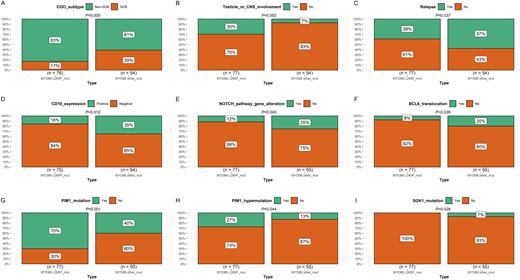
Results: A total of 132 DLBCL patients with MYD88 mutation were included in the study, among which 58% (77/132) occurred MYD88 L265P mutation, while 42% (55/132) were MYD88 other variants. We found that MYD88 L265P mutation and other variants showed statistically significant distribution in COO subtype, testicle/CNS involvement, disease relapse, CD10 expression, BCL-6 translocation, NOTCH pathway gene alteration, PIM1 mutation, PIM1 hypermutation, and SGK1 mutation (Figure 1). Specifically, MYD88 L265P variant was more common seen in non-GCB subtype than other variants (83% vs. 61%, P=0.005). Besides, MYD88 L265P variant was significantly related to higher proportion of testicle/CNS involvement (30% vs. 7%, P=0.002), PIM1 mutation (70% vs. 40%, P<0.001), and PIM1 hypermutation (27% vs. 13%, P=0.044), compared with other variants. Instead, MYD88 other variants were more likely to have higher percentage of disease relapse (57% vs. 39%, P=0.037), positive CD10 expression (35% vs. 16%, P=0.012), BCL-6 translocation (20% vs. 8%, P=0.039), SGK1 mutation (7% vs. 0%, P=0.030), and NOTCH pathway gene alteration (25% vs. 12%, P=0.040), compared with MYD88 L265P mutation.
Conclusion: Our findings indicated that DLBCL patients with MYD88 L265P mutation and other variants are likely to be two subgroups with different clinical and molecular characteristics.
Keywords: DLBCL; MYD88 mutation
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal